Perimetry Test Results. Unlike central vision acuity which is measured by what letter size can be seen from a given distance, visual field testing measures the threshold of vision in decibels (dB). A smaller distinguishable stimulus threshold equates to more sensitive vision detection. These results are depicted using dB numbers for the area of peripheral vision being measured. The dimmer the light stimulus visible to the patient, the more sensitive the vision is for that particular point in the field of vision. Perimetry usually tests dozens of different visual points. Here are common ways the data is analyzed and depicted.
Numerical plot: Displays the threshold for all visual points tested.
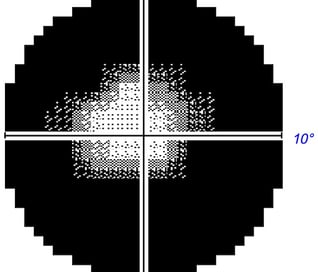
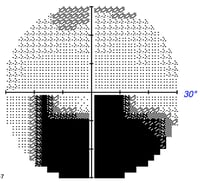
Grayscale plot: Graphically depicts visual field loss. Normal areas are white and affected areas are grey/black. The level of darkness denotes the magnitude of vision loss for that area with darker being more severe.
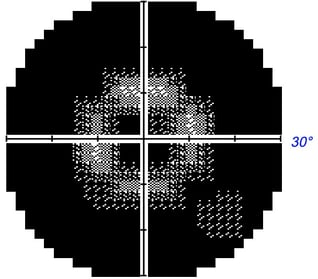
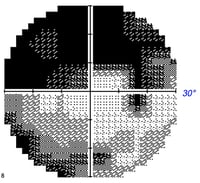
Total deviation plot: Compares the patient’s results with normal age-matched controls and graphs areas of potential vision loss. This data can be influenced by extraneous factors though (ex. cataracts).
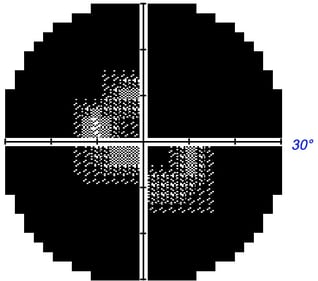
Pattern deviation plot: Similar to the total deviation plot except this is adjusted for any generalized depression seen on the total deviation plot. This is helpful with conditions affecting all visual points (ex. cataracts).
Mean deviation: An average of the results from all tested locations and compared with normal values.
Pattern standard deviation: Provides data about localized rather than generalized visual field loss.
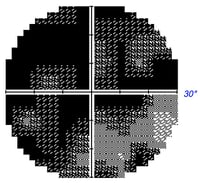
Hemifield test: Compares visual field loss of the upper hemifield to the lower hemifield. This is especially useful with glaucoma suspects.
Many forms of visual field defects exist corresponding with different ocular and neurological conditions. For instance, a bitemporal hemianopia is associated with a pituitary gland tumor of the optic chiasm while an enlarged blind spot is an indicator of optic neuritis.
Perimetry Interpretation. As with all medical diagnostic assessments, the data interpretation and disease management need to be determined by a trained professional. Having said that, there are some basic fundamentals non-professional may use to roughly interpret perimetry results. Before testing should be interpreted, one must ensure the test results are reliable (discussed in greater detail in the next section).
Firstly, each eye should have a blind spot that corresponds with the optic nerve head as this area of the eye does not detect light, but carries information to the brain from other areas of the retina. If the blindspot is missing, the contralateral eye may not have been appropriately covered.
The gray scale plot (usually at the top) is a way to quickly visualize and generally assess peripheral vision loss. Though the gray scale is a great starting point, it is not always accurate. The gray scale also reveals which eye has been evaluated – if the blind spot is on the left then the left eye was evaluated; if the blind spot is on the right the right eye was evaluated.
The mean deviation analyzes and quantifies if the eye has above average sensitivity (positive number), average sensitivity (zero), or reduced sensitivity (negative number). The more negative the number, the greater the overall vision loss for that eye. A high pattern standard deviation number reveals if there is a significant difference between the upper and lower hemifield, which is especially useful in glaucoma evaluation. This can easily be interpreted by looking at the glaucoma hemifield test (GHT) that simply states if this is within normal limits, borderline, or outside normal limits.
The total deviation plot displays the total magnitude and location of vision loss; remember this can be affected by media opacities (cataracts, corneal scars, vitreous hemorrhages, etc). Usually considered more useful is the pattern standard deviation plot, which displays the vision loss after taking into account the total deviation.


.jpeg)

-1.jpeg?width=640&name=Importe%20-%201%20von%201%20(7)-1.jpeg)

.jpeg)
.jpeg?width=499&name=Alle%20Fotos%20-%201%20von%201%20(5).jpeg)

.jpeg?width=393&name=Importe%20-%201%20von%201%20(6).jpeg)
.jpeg?width=640&name=Importe%20-%201%20von%201%20(21).jpeg)
.jpeg)

.jpeg?width=200&name=Importe%20-%201%20von%201%20(11).jpeg)
.jpeg?width=200&name=Importe%20-%201%20von%201%20(12).jpeg)
.jpeg?width=200&name=Importe%20-%201%20von%201%20(13).jpeg)

.jpeg?width=200&name=Importe%20-%201%20von%201%20(15).jpeg)
.jpeg?width=250&name=Importe%20-%201%20von%201%20(16).jpeg)