 My name is Khanh, and I’m 33 years old from Vietnam. My journey to recovery began after what was supposed to be a simple vision correction surgery for high myopia. Instead, it turned into a nightmare that changed my life. The surgery, which involved laser correction, caused complications that led to a dangerous rise in my eye pressure. This triggered secondary glaucoma—a condition where high intraocular pressure damages the optic nerve. Over time, my vision became increasingly blurry, and I struggled with even the most basic daily tasks. At my lowest point, I could barely read a text message or see everyday objects clearly. It felt like my independence and quality of life were slipping away.
My name is Khanh, and I’m 33 years old from Vietnam. My journey to recovery began after what was supposed to be a simple vision correction surgery for high myopia. Instead, it turned into a nightmare that changed my life. The surgery, which involved laser correction, caused complications that led to a dangerous rise in my eye pressure. This triggered secondary glaucoma—a condition where high intraocular pressure damages the optic nerve. Over time, my vision became increasingly blurry, and I struggled with even the most basic daily tasks. At my lowest point, I could barely read a text message or see everyday objects clearly. It felt like my independence and quality of life were slipping away.
Understanding My Condition
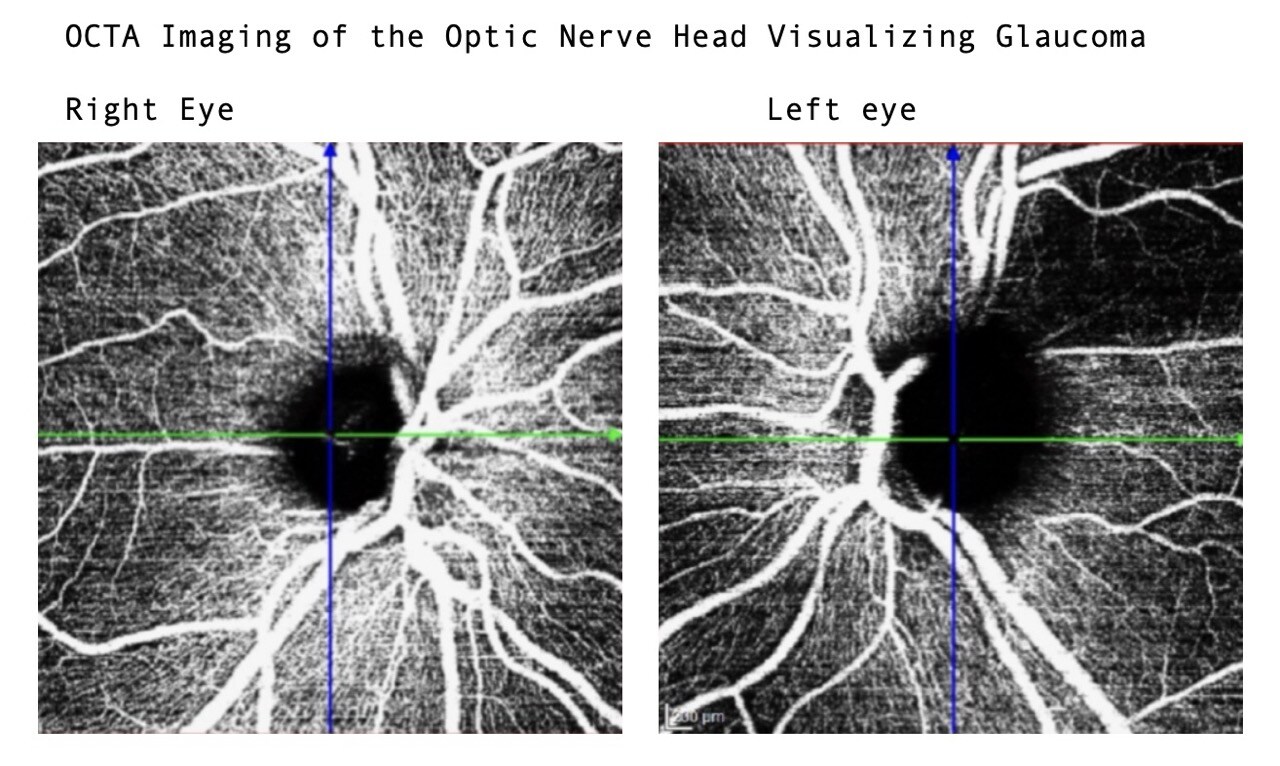
My doctors explained that my glaucoma wasn’t the typical kind; it was a secondary form caused by complications from laser surgery. High myopia had already made my eyes vulnerable, and the surgical aftermath caused my intraocular pressure to rise uncontrollably. This led to gradual optic nerve damage in both eyes. By the time I sought help, the damage was already severe.
According to my medical records, the cup-to-disc ratio in my right eye was as high as 0.9, which meant that most of my optic nerve fibers were gone. My left eye, though slightly better, was also at risk. The high pressure in my eyes caused headaches, strain, and a constant feeling of foggy vision. It was like looking at the world through a frosted window.
Daily Life with Vision Loss
Living with such limited vision was incredibly challenging. Everyday tasks became impossible without assistance.
- Navigating My Surroundings: Walking alone was terrifying. I couldn’t see obstacles clearly and often tripped or bumped into objects. Crossing the street without help was out of the question.
- Household Tasks: Cooking felt dangerous. I would burn myself on hot pots or spill boiling water because I couldn’t judge distances. Cleaning and organizing were equally difficult—I couldn’t even tell if a surface was clean or cluttered.
- Social Life: Recognizing faces was one of the hardest things. Meeting friends or family felt awkward because I couldn’t tell who was in front of me until they spoke. It was isolating, and I found myself withdrawing from social interactions.
- Reading and Technology: I relied entirely on audio tools because reading even large print was impossible. Sending a text message or checking emails became monumental tasks.
Turning Point: Finding Hope at Fedorov Restore Vision Clinic
At my lowest point, I felt hopeless. My vision was so poor that I thought I would never regain any independence. Then I discovered the Fedorov Restore Vision Clinic, and everything changed. Their approach focused on improving vision through electrical stimulation therapy, which gave me a chance to regain some clarity despite the severe damage to my optic nerves.
After my first round of treatment, I started to see subtle but life-changing improvements. I could cross the street independently for the first time in years—a milestone I thought I’d never reach again. Over the course of three rounds of treatment, my vision improved significantly. Now, I can read standard text, walk down stairs comfortably, and live a normal daily life without needing support.
How My Doctors Helped Me Understand the Process
My doctors emphasized that secondary glaucoma is a complex and progressive condition. They explained that while surgeries like trabeculectomy helped lower my intraocular pressure, the optic nerve damage was permanent. The staff at Fedorov Restore Vision Clinic explained that their treatment aimed to stimulate the remaining healthy nerve fibers, improving visual function and slowing further deterioration.
Their transparency was reassuring—they were clear that while major improvements weren’t guaranteed, even small changes could transform my quality of life. After three rounds of treatment, I can confidently say that their efforts exceeded my expectations.
Analysis of Visual Field Improvements Following Fedorov Restoration Therapy
The following section presents an in-depth analysis of Khanh’s visual field (VF) results, highlighting the positive impact of Fedorov Restoration Therapy on her functional vision. These results demonstrate measurable recovery in her visual capacity, reflecting both structural stabilization and enhanced visual function. This analysis will showcase how the therapy contributed to slowing the progression of glaucomatous damage and improving her quality of life.
30-Degree Visual Field (Right Eye) |
|
|
July 18, 2022 |
October 14, 2024 |
.jpeg?width=640&height=580&name=Glaucoma%20vision%20improvement%20Fedorov%20Restore%20Vision%20Clinic10.24.08).jpeg)
|
.jpeg?width=640&height=580&name=Glaucoma%20vision%20improvement%20Fedorov%20Restore%20Vision%20Clinic10.23.58).jpeg)
|
|
• VFI (Visual Field Index): 14% |
• VFI: 38% |
30-Degree Visual Field (Left Eye) |
|
.jpeg?width=640&height=580&name=Glaucoma%20vision%20improvement%20Fedorov%20Restore%20Vision%20Clinic10.24.36).jpeg)
|
.jpeg?width=640&height=580&name=Glaucoma%20vision%20improvement%20Fedorov%20Restore%20Vision%20Clinic10.24.18).jpeg)
|
|
• VFI (Visual Field Index): 22% |
• VFI: 49% |
Clinical SummaryRight Eye (RE) Left Eye (LE) |
|
Life Today: Independence Restored
What Khan is saying: ... Today, I can do things I thought were lost to me forever. I can walk through busy streets without fear, read books and text messages, and navigate stairs and uneven terrain with ease. These may seem like small things, but for someone who once couldn’t distinguish a face or walk unassisted, they are life-changing.
The warm and compassionate care from the team at Fedorov made all the difference. Their unwavering support gave me the strength to keep going, even when progress felt slow. Traveling halfway across the world for this treatment was a leap of faith, but it was the best decision I ever made.
My Message to Others
If you’re living with glaucoma or struggling with vision loss, know that there is hope. The journey is not easy, and the road to improvement may feel long, but with the right care and determination, progress is possible. The team at Fedorov Restore Vision Clinic didn’t just restore my vision—they restored my confidence and hope for the future.
If my story resonates with you, I encourage you to seek help and never stop fighting for your independence. Life can be beautiful again.
Khan's story published here: https://www.restorevisionclinic.com/success-story-secondary-glaucoma-fedorov-therapy-vision-restoration
Expert Opinions: Navigating the Risks of Refractive Surgery and Glaucoma
Refractive Surgery and Secondary Glaucoma: A Critical Overview
Refractive surgery can dramatically improve vision, offering a life-changing alternative to glasses or contact lenses. However, it is not without risks, particularly for individuals predisposed to glaucoma. Secondary glaucoma—a condition caused by elevated intraocular pressure (IOP) that damages the optic nerve—can be a rare but serious complication. Patients should be aware of these risks and take steps to ensure informed decisions and proper care.
Understanding the Risks Across Procedures
LASIK, a widely performed refractive surgery, has an overall complication rate of less than one percent. Despite this, it can lead to secondary glaucoma through several mechanisms. Post-operative steroid use can elevate IOP in approximately 30% of patients, particularly those who are sensitive to corticosteroids. Intraocular pressure can spike during the creation of the corneal flap, reaching levels as high as 60–90 mm Hg. While these spikes are temporary, they can cause lasting damage in individuals with pre-existing optic nerve vulnerabilities. Additionally, the thinning of the cornea after LASIK can mask true IOP readings, delaying glaucoma diagnosis. Rare complications such as Pressure-Induced Interlamellar Stromal Keratitis (PISK) and interface cysts can further complicate management.
Other procedures, such as PRK and SMILE, have slightly lower risks of secondary glaucoma. PRK avoids creating a corneal flap, reducing IOP spikes, but post-operative steroid use remains a concern. SMILE, a newer procedure, preserves corneal biomechanics, potentially reducing risk, although long-term data are still limited. Phakic Intraocular Lenses (pIOLs), used for high myopia, carry a 2–6% risk of secondary glaucoma, often due to angle-closure complications or anatomical changes. Refractive Lens Exchange (RLE), often performed for extreme myopia or presbyopia, has a 5% risk, primarily due to structural disruptions caused during surgery.
The Importance of a Pre-Surgical Checklist
A comprehensive pre-surgical assessment is essential for identifying at-risk individuals and ensuring the safest surgical approach. The following checklist highlights critical risk factors for secondary glaucoma:
- High Myopia or Hyperopia: Myopia increases glaucoma risk two- to four-fold due to anatomical predispositions, such as thinner sclera and weaker optic nerve support.
- Family History of Glaucoma: A genetic predisposition can significantly elevate risk, even in the absence of other factors.
- Age Over 40: Aging increases susceptibility to glaucoma due to natural degeneration of optic nerve structures.
- Previous or Current Elevated IOP: A history of ocular hypertension or steroid-induced IOP elevation may indicate a higher risk.
- Thin Central Corneas: Thin corneas can mask true IOP levels, leading to delayed detection of glaucoma.
- Ethnicity: Individuals of African, Hispanic, Latino, or Asian descent have higher rates of glaucoma, making risk assessments particularly important.
- Systemic Conditions: Diabetes, cardiovascular disease, and obstructive sleep apnea are known to increase glaucoma risk.
- Use of Steroids: Long-term corticosteroid use, including eye drops, inhalers, or systemic steroids, can elevate IOP and should be disclosed.
- History of Eye Surgery or Injury: Prior ocular trauma or surgery can increase vulnerability to complications.
Each of these factors plays a critical role in assessing a patient’s risk. For instance, thin central corneas make it difficult to accurately measure IOP, a cornerstone of glaucoma management. High myopia and systemic conditions can exacerbate optic nerve vulnerability, while family history or ethnic background may predispose individuals to disease even without additional risk factors.
Why This Matters Patients checking multiple boxes in this checklist are at higher risk for secondary glaucoma and should consult their ophthalmologist for tailored recommendations. A detailed evaluation of the optic nerve, IOP levels, and corneal thickness can inform the choice of the safest procedure. For some high-risk individuals, alternative corrective strategies or additional monitoring post-surgery may be required to prevent complications.
Connecting with Real-Life Stories Khanh’s story demonstrates the profound impact secondary glaucoma can have after refractive surgery. Despite severe vision loss due to complications, advanced therapies and careful management enabled her to regain independence and improve her quality of life. His experience highlights the importance of understanding risks, undergoing thorough evaluations, and exploring innovative treatments when necessary.
Conclusion: Making Safe and Informed Choices While refractive surgery offers high satisfaction rates and significant quality-of-life improvements, understanding potential complications like secondary glaucoma ensures patients make safer decisions. Pre-surgical checklists, comprehensive evaluations, and informed discussions with an experienced ophthalmologist are essential for minimizing risks. By taking these precautions, patients can enjoy the benefits of refractive surgery while safeguarding their long-term vision health.
List of key publications:
1. Xu L, Wang Y, Wang S, et al. High myopia and glaucoma susceptibility: the Beijing Eye Study. Ophthalmology. 2007;114(2):216-220[1].
2. Marcus MW, de Vries MM, Junoy Montolio FG, Jansonius NM. Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology. 2011;118(10):1989-1994[1].
3. Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042[5].
4. Goyal S, Khaw PT. Refractive Surgery: A Glaucoma Specialist's Perspective. CRST Europe. 2010[1].
5. Shalaby WS, Khoueir Z, Chia SH, et al. Refractive surgery for the glaucoma suspect. Curr Opin Ophthalmol. 2023;34(4):321-327[2].
6. Bashford KP, Shafranov G, Tauber S, Shields MB. Considerations of glaucoma in patients undergoing corneal refractive surgery. Surv Ophthalmol. 2005;50(3):245-251[3].
7. Chihara E, Tanihara H. Parameters associated with papillomacular bundle defects in glaucoma. Graefes Arch Clin Exp Ophthalmol. 1992;230(6):511-517[3].
8. Shalaby WS, Khoueir Z, Chia SH, et al. The Effect of Corneal Refractive Surgery on Glaucoma. J Ophthalmol. 2017;2017:1649268[3].
9. Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714-720[3].
10. Medeiros FA, Sample PA, Weinreb RN. Corneal thickness measurements and visual function abnormalities in ocular hypertensive patients. Am J Ophthalmol. 2003;135(2):131-137[3].
Disclaimer The information provided in this blog is for educational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. While every effort has been made to ensure the accuracy and reliability of the information, readers should consult with a qualified ophthalmologist or healthcare professional before making decisions about refractive surgery or glaucoma management. The potential risks and complications of refractive surgeries, including secondary glaucoma, vary significantly based on individual factors such as pre-existing medical conditions, family history, and the type of surgical procedure chosen. This blog aims to provide general guidance and raise awareness but cannot account for every individual circumstance or medical nuance. If you are considering refractive surgery or have concerns about your eye health, it is essential to undergo a comprehensive evaluation by an experienced eye care provider. This includes detailed assessments of your intraocular pressure, optic nerve health, and corneal thickness, as well as an analysis of your personal risk factors. The authors and publishers of this blog do not accept liability for any decision made or action taken based on the content provided herein. Always seek the advice of a licensed healthcare provider with any questions regarding a medical condition or surgical procedure. Never disregard professional advice or delay seeking treatment based on information provided in this or any other online resource.




Comments
Currently, there are no comments. Be the first to post one!