INTRODUCTION
Identified as early as 1884 by Magnus, optic nerve hypoplasia (ONH) is a congenital malformation consisting of small, underdeveloped optic discs causing visual impairment from birth. ONH is non-progressive and varies widely in severity, ranging from near normal central visual acuity to no-light perception in severe cases. Though typically found bilaterally, ONH may be present unilaterally as well. ONH accounts for approximately 15-25% of severe vision loss in infants and, when bilateral, 80% of patients fall into the classification of legal blindness.

ONH may occur in isolation, but is usually associated with other ocular, facial, or intracranial abnormalities. Early research identified a connection between ONH and agenesis of the septum pellucidum leading to a commonly referenced diagnosis of septo-optic dysplasia (de Morsier’s Syndrome), which affects both optic nerve and midbrain development. Both ONH and septo-optic dysplasia arise from miswiring and diminished number of axons leading to impaired function of affected structures. While possible, ONH rarely occurs in the absence of functional or anatomical neurological disorders, the most common of which being pituitary and hypothalamus maldevelopment.
Previously believed to be exceedingly rare, ONH incidence is rising, possibly due to associations between ONH and brain malformations being better understood. Prior to 1970, English literature had reported fewer than 30 cases. In the early 1980’s research conducted in Houston, Texas found ONH in 12% of blind infants. By 1997 ONH had become the leading cause of infant blindness in Sweden and, between 1980-1999, the incidence of ONH had increased fourfold to 7.2 per 100,000 in Sweden. Similarly, the prevalence of ONH in England has risen to 10.9 per 100,000 as of 2006. Though the upsurge of ONH diagnoses could be attributed to improved recognition and sensitivity, this is doubtful as ONH is usually easily discernible with direct ophthalmoscopy and the escalating occurrence is being reported from the same institutions. This new data repudiates the previously assumed paucity of ONH.
PRENATAL RISK FACTORS
General
All ethnicities are affected by ONH, but there appears to be a slightly lower prevalence amongst Asian populations. No gender predilection has been revealed either.
Genetic
While specific genetic mutations have been demonstrated to impact optic nerve development, only one gene (HESX1) is known to impact both optic nerve and pituitary development. However, the HESX1 genetic mutation is found in less 1% of ONH cases, and is therefore an unlikely cause. No specific genotype or phenotype correlations have been identified.
Gestational and Exposure History
A myriad of prenatal and perinatal risk factors have been reported for ONH including preterm birth, low birth weight, intrauterine growth restriction, twin-twin transfusion syndrome, young maternal age, and primiparity. Certain prenatal complications raise the risk of ONH such as gestational diabetes, toxemia, maternal anemia, and viral infections. Prenatal exposure to smoking, alcohol, infertility treatments also may further the chance of ONH occurrence.
The only well-established maternal characteristics connected with ONH are maternal age, primiparity, and gestational diabetes – the latter of which being associated with a specific form of ONH known as superior segmental ONH. No lifestyle factors have been conclusively linked with ONH and the role of nutrition has not been carefully evaluated.
INHERITANCE
Research has demonstrated that ONH is not inherited, but rather sporadically occurring. Family members of those with ONH are not at increased risk. However, some familial cases of septo-optic dysplasia may have an autosomal-recessive pattern, and a few cases have noted an autosomal-dominant pattern.
DIAGNOSIS

ONH is easily distinguishable with direct ophthalmoscopy in moderate to advanced cases of ONH. While having a somewhat similar appearance to optic atrophy, careful ophthalmological examination may oftentimes differentiate optic nerve hypoplasia from optic nerve atrophy. Diagnosis is far more difficult in mild cases of ONH as the hypoplastic nerve is less appreciable.
The most notable sign of ONH is a small, underdeveloped optic disc where the calculated disc area may be anywhere from 39-93% of a normal disc area. A classic indicator of ONH is the “double ring sign” visualized as a pigmented peripapillary ring surrounding a hypopigmented area around the optic nerve. The white hypopigmented area is the underlying exposed sclera while the pigmented area is presumed to occur from migration of pigmented epithelium and sensory retina to the border of the optic nerve from the usual edge of the optic stalk. The hyperpigmented border adjacent to the exposed white sclera forms this “double ring sign”. The optic disc may also present as slightly gray or even white in color.
Another characteristic of ONH is an increased optic disc to macula diameter. The normal disc to macula diameter is approximately 3 optic disc diameters in length, while ONH afflicted eyes usually have a larger disc to macula diameter approximating 4 optic disc diameters. Interesting, eyes with ONH typically have retinal vessels (arterioles, venules, or both) appearing either unusually tortuous or unusually straight with decreased branching. The macula also may have a flattened contour resulting in loss of the traditional foveal light reflex.
There is no single, pathognomonic sign indicating ONH. Vascular tortuosity may be increased or decreased. The double ring sign is not always present. The disc area may be as great as 93% of the normal disc size, which is essentially indistinguishable from a normal optic nerve. Nerve fiber layer loss may not be discernable solely with ophthalmoscopy. Furthermore, cases of mild ONH may be exceedingly challenging to detect thus requiring additional objective diagnostic methods, such as optical coherence tomography (OCT) or magnetic resonance imaging (MRI). Recent studies revealed that scans of the visual pathways using MRI technology serves as a better diagnostic tool than ophthalmological evaluation of the optic discs, especially in mild ONH cases. Additionally, Brodsky and Glasier developed an ONH classification system based on MRI scans of the central nervous system capable of predicting the risks of neurodevelopmental deficits and endocrinologic dysfunction in individuals.
OPTICAL COHERENCE TOMOGRAPHY
Optic nerve hypoplasia (ONH) is a non-progressive, congenital abnormality of one or both optic nerves associated with a diminished number of optic nerve axons, but with normal development of supportive tissues and a functional retinal vascular system. This reduced number of axons can be observed with ophthalmoscopy by a smaller than normal optic disc size. The retinal nerve fiber layer (RNFL), inner retinal layers (IRL), and ganglion cell numbers are diminished, yet the outer retinal layers (ORL) remain unaffected.
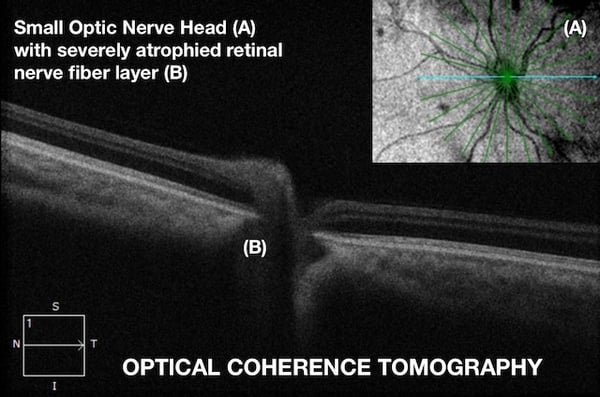
OCT is non-invasive, in vivo, imaging of the optic nerve and retina (particularly the macula), which provides accurate, reproducible, high-definition, cross-sectional scans. This technology is capable of visualizing and measuring the thickness of individual retinal layers. For this reason, OCT proves to be diagnostically invaluable in ONH as it provides in-depth information of the optic disc, RNFL, IRL, and ORL.
In ONH, congenital deficiency of retinal ganglion cells and axons leads to disorganization of the retinal ganglion cell layer, thinning of RNFL, and a small optic disc. While the pathogenesis is not fully understood, ONH is thought to occur due to insult(s) to the visual pathway, especially in early development, before complete development of the visual system.
While diagnosis of ONH primarily is made clinically through ophthalmoscopy, accurate diagnosis becomes problematic when the degree of hypoplasia is less severe or even segmental in nature, because the RNFL thinning and disc underdevelopment may be indiscernible solely with ophthalmoscopy.
Therefore, OCT is a vital diagnostic instrument as it provides accurate, quantitative, detailed, and reproducible measurements of the optic nerve and macula. OCT is the standard of care in diagnosing and management of optic nerve and retinal anomalies. Nevertheless, there have been few reports on detecting ONH using OCT worldwide. In our patient population, the clinical characteristics of the optic nerve head reveal typical features of ONH. Our data obtained through SD-OCT and manual segmentation demonstrates thinning of the RNFL and IRL with preserved ORL in our patients with congenital, unilateral ONH, which coincides with a conventional histological report.
OPTIC NERVE HEAD TYPES
ONH has been divided into three clinical subtypes based on the presence of neurological complications.
Type I: Optic Nerve Hypoplasia Simplex
- Diffuse
- Segmental
- Segmental with tilt
Type II: Septo-optic Dysplasia
Type III: Septo-optic Pituitary Dysplasia
Type II and Type III are differentiated by the additional component of hypopituitarism associated with Type III. Type I also includes a form of ONH associated with gestational diabetes termed Superior Segmental Optic Nerve Hypoplasia or topless disc syndrome.
OCULAR ASSOCIATIONS AND SYMPTOMS
Roughly 80% of ONH cases are bilateral in nature. Unless accompanied by systemic complications, unilateral ONH is typically diagnosed at a later age due to better overall vision. Central visual acuity ranges from almost normal to no light perception, however legal blindness is found in more than 80% of bilateral cases. Interestingly, there is little to no evidence correlating visual acuity with optic disc size.

Numerous ocular abnormalities may present in conjunction with ONH, the most common of which being microphthalmos, aniridia, albinism, chorioretinal coloboma, nystagmus, strabismus, and high myopia. In cases of bilateral ONH, nystagmus may develop between 1-3 months of age. Strabismus occurs more frequently in unilateral ONH and usually appears in the first year of life. Peripheral vision and depth perception are often affected, especially in children with severe vision loss. Parents also may notice light avoidance and mild photophobia in kids with ONH.
Visual acuity oftentimes marginally improves in the first few years of life. Although the reason is uncertain, this may be due to improved axonal function and optic nerve myelination, which occurs until age 4. ONH is a non-progressive condition and worsening vision has never been reported.
SYSTEMIC ASSOCIATIONS AND SYMPTOMS
While ONH may occur in isolation, it frequently is accompanied by neurological or hormonal complications.
NEUROLOGICAL
ONH is often associated with cranial malformations of midline brain structures, especially the septum pellucidum. As mentioned before, ONH is often linked with septo-optic dysplasia or deMorsier’s Syndrome. Hypoplasia of the optic nerves, reduced function of midline brain structures, and underdevelopment of the pituitary gland characterizes septo-optic dysplasia. Agenesis of the septum pellucidum is found in 27% of patients with ONH. Similarly, ONH is seen in 25% of patients with agenesis of the septum pellucidum. Signs of septo-optic dysplasia are impaired cognition, spasticity, and impaired sense of taste and smell. Complications arising from midline brain maldevelopment may include anencephaly, cerebral atrophy, basal encephaloceles, hypoplastic cerebellar vermis, cystic dilation of the 4th ventricle, posterior fossa cysts, and space occupying lesions of the anterior visual pathway. Developmental delays are seen in 39% of unilateral ONH patients and 79% of bilateral ONH patients. Cerebral palsy is estimated to occur in roughly 13% of ONH cases.
HORMONAL
Hypothalamic and pituitary dysfunction occurs in 69% of unilateral ONH cases and 81% of bilateral ONH cases. Hormonal insufficiencies or imbalances may be discovered in childhood or may not present until later in life. All pituitary hormones may be affected and hypopituitarism is found in approximately 75% of ONH patients.
Some symptoms of pituitary imbalance include increased fatigue and irritability, circadian rhythm dysfunction, short stature, delayed puberty, seizures, abnormal hunger or thirst, impaired temperature regulation, prolonged jaundice, and hypoglycemia. Hormonal deficiencies may occur without evidence of brain malformations, but are more frequent in bilateral ONH cases and in kids with observable midline brain defects.
DEVELOPMENT
ONH is frequently accompanied by developmental delays, encompassing a broad clinical spectrum and ranging from isolated focal defects to large-scale delays. Standardized testing data reveals adverse developmental outcomes in 71% of ONH patients. Motor delays occur most frequently at a rate of 77% while communication delays are the least common affecting 44% of these children. Neuropsychiatric disorders are present in approximately 75% of ONH patients. Developmental delays are found with both unilateral and bilateral ONH, but are almost twice as likely to occur in bilateral cases.

ELECTROPHYSIOLOGY
Photoreceptors, located in the outer retina, are unaffected by ONH resulting in normal electroretinograms (ERGs) and electrooculograms (EOGs). Conversely, flash visual evoked potentials (fVEP), which measures respond of visual cortex of the brain when eye was stimulated with bright flash, have reduced amplitude as a the result of optic nerve and visual pathway abnormality, Few ocular conditions have normal ERGs and EOGs, yet abnormal VEPs. Major benefits of electrophysiologal examinations for kind is to establish amount of preserved vision in case when routine tests are not applicable due to the young age of the patients. Therefore, electrophysiology is of diagnostic significance and may differentiate ONH from similarly presenting congenital conditions such as Leber’s Hereditary Optic Neuropathy and achromatopsia
NEUROIMAGING

While high-resonance MRI is useful in distinguishing ONH from optic atrophy, MRI is also useful is the diagnosis of ONH, especially in mild cases which have proved difficult to diagnose with ophthalmoscopy alone. Small optic nerves in conjunction with septum pellucidum agenesis, corpus callosum hypoplasia, and pituitary malformations are suggestive of ONH. The septum pellucidum is partially or completely absent between 27-38% of ONH cases. MRI is especially helpful in predicting future hormonal deficiencies as studies have revealed that children have an increased risk of pituitary dysfunction when both the septum pellucidum is absent and maldevelopment of the pituitary gland occurs. Absence of the septum pellucidum in isolation does not have any predictive value for hypopituitarism, developmental difficulties, or adverse outcomes. However, hypopituitarism may still occur in the presence of a normal septum pellucidum and pituitary gland as demonstrated by a high rate of hypopituitarism amongst ONH patients but only 13% of these children having an abnormal MRI scan. Another brain structure potentially underdeveloped in ONH kids is the corpus callosum. Hypoplasia of the corpus callosum negatively affects development of cognitive, motor, and adaptive behavioral skills. Other midline structural abnormalities seen with MRI, which affect less than 15% of ONH patients, may lead to schizencephaly, cortical heterotopia, white matter hypoplasia, pachygyria, and holoprosencephaly.
MANAGEMENT AND RECOMMENDATIONS
The syndrome of optic nerve hypoplasia is known to be a miswiring of axons in the optic nerve often associated with miswiring elsewhere in the brain, especially the hypothalamus and midline structures. Therefore it is medically prudent for physicians to be cognizant and vigilant for signs and symptoms affecting vision, cognitive development, behavior development, and hormonal function.
Children with prolonged neonatal jaundice, recurrent hypoglycemia, or temperature instability are recommended to have an ophthalmological examination. Any child potentially demonstrating poor visual function, nystagmus, or strabismus should have a comprehensive eye examination by 3 months of age. Additionally, if an MRI reveals midline brain anomalies, an ophthalmological examination is necessitated. (Image)
In cases where ONH is diagnosed or suspected, an MRI and endocrinologic evaluation is warranted. Such results may provide insight on related and treatable conditions as well as help predict potential developmental and hormonal deficiencies. Children should be monitored twice a year for growth and endocrinologic studies.
Medical professionals should have enhanced monitoring of developmental skills and awareness for the potential need of occupational, physical, and speech therapy. Parents should be educated about possible sleep dysregulation in these children and treatment should be initiated if circadian dysfunction ensues.
Eye examinations should be conducted at least annually to properly correct refractive errors, manage strabismus and amblyopia, and treat any other ocular conditions present.
Parents or caregivers should be thoroughly educated on ONH and any associated conditions present as well the prognosis and developmental expectations. As ONH may cross into multiple specialties, enhanced communication between medical specialties is necessary to ensure optimal patient care.
CONCLUSIONS
Relating to the miswiring and maldevelopment of the central nervous system, the diagnosis of ONH has broad implications impacting ocular, neurological, and hormonal systems. Often first detected through ophthalmological evaluation, management of ONH requires a multidisciplinary approach and meticulous management due to frequently associated endocrinopathy, brain malformations, and developmental delays. Although no cure for ONH exists, timely intervention may minimize the impact of vision loss and generally improve development in these children.
FEDOROV RESTORATION THERAPY
An underdeveloped optic nerve is a congenital problem, leading to eyesight deterioration. Fedorov Therapy is meant to help your kid to regain eyesight naturally. Because children's brains are more easily molded, our therapy is directly beneficial to improving their visual acuity, contrast vision and enlarge field of vision.
Real-Life Inspiration: Kristián’s Journey with ONH: Kristián, a young boy born with optic nerve hypoplasia (ONH), is living proof of how tailored therapies can make a significant difference. After beginning Fedorov Restoration Therapy at our clinic in Berlin, he has made remarkable progress. Kristián can now recognize shapes, colors, and objects, walk independently, and confidently navigate his surroundings—all achievements that were once unimaginable.
His story highlights the potential of our personalized approach to support visual function and improve daily life for those living with ONH. Learn more about Kristián’s inspiring journey and how our therapies help patients unlock their potential.
Blog prepared in cooperation with Kaleb Abbott, O.D., M.S.
REFERENCES
- Borchert M, Garcia-filion P. The syndrome of optic nerve hypoplasia. Curr Neurol Neurosci Rep. 2008;8(5):395-403.
- Kaur S, Jain S, Sodhi HB, Rastogi A, Kamlesh . Optic nerve hypoplasia. Oman J Ophthalmol. 2013;6(2):77-82.
- Dutton GN. Congenital disorders of the optic nerve: excavations and hypoplasia. Eye (Lond). 2004;18(11):1038-48.
- Frisén L, Holmegaard L. Spectrum of optic nerve hypoplasia. Br J Ophthalmol. 1978;62(1):7-15.






4 Comments
Click here to read/write comments