CAUSES OF OPTIC NERVE NEUROPATHY
Now that we’ve examined a variety of symptoms of optic nerve neuropathy, it’s time to take a more detailed look at many of the most common causes of optic nerve neuropathy, many of which were briefly mentioned above, and all of which are quite serious and require immediate attention and thorough treatment.
Now that we’ve examined a variety of symptoms of optic nerve neuropathy, it’s time to take a more detailed look at many of the most common causes of optic nerve neuropathy, many of which were briefly mentioned above, and all of which are quite serious and require immediate attention and thorough treatment.
Glaucoma: Glaucoma is one of the most common causes of optic nerve damage and subsequent vision loss, which is often the first sign of the condition due to the fact that, generally, glaucoma causes no pain until the condition has advanced considerably. One of the leading causes of blindness worldwide, glaucoma is commonly related to ocular hypertension, or increased pressure within the eye.
There are two subtypes of glaucoma associated with high intraocular pressure— - open-angle glaucoma and closed-angle glaucoma, the former being the far more commonly occurring variety. Open-angle glaucoma progresses slowly, and, again, generally produces no pain. As it develops, glaucoma gradually reduces one’s field of vision (or peripheral vision), while central vision is preserved for a longer time. However, the end stages of developed terminal glaucomatous optic nerve damage leads to total blindness.
It’s important to mention that vision loss is not always associated with elevated intraocular pressure. Some glaucoma patients develop typical symptoms of eyesight loss where elevated pressure cannot be revealed, which is generally known as normal-tension glaucoma.
Glaucoma is usually diagnosed during an eye exam by using instruments that test the intraocular pressure within the eye, field of vision, and thickness of the optic nerve. Once diagnosed, proper treatments, such as surgery, medications, specialized eye drops, or laser procedures, will be administered. The proper glaucoma management for each case of the condition is often determined by success in lowering of intraocular pressure, the speed of glaucomatous optic nerve damage, and the timing of vision loss.
Lack of Blood Supply (Ischemic Optic Neuropathy): Ischemic optic neuropathy is a condition in which a lack of blood supply results in damage to the optic nerve and subsequent loss of vision. The majority of all ischemic optic neuropathies are anterior ones (AION), meaning blood vascularization in the optic nerve occurs close to the eyeball. This is usually due to inflamed arteries, or arteric AION. By contrast, the most frequent conditions of AION are non-arteric (NAION), in which the lack of blood supply is due to non-inflammatory causes.
The onset of NAION is often rapid and painless, commonly experienced upon waking due to a drop in blood pressure during sleep, and generally causes part or half of an individual’s vision to become obscured or impaired. Full vision loss occurs in some cases but is exceedingly rare. Three major causes of NAION have been determined: first, an optic disc that is too narrow to accommodate the optic nerve from which it emerges; second, sleep apnea syndrome and third, various cardiovascular conditions including high cholesterol, diabetes, and hypertension. However, the aforementioned fall in blood pressure overnight is the most common cause. Patients are generally diagnosed via an eye examination and consideration of other health factors and predispositions. Treatment of the condition has often been difficult, although some specialized treatments using certain types of steroids can be partially successful.
Eye or Head Trauma: Any type of trauma or injury to the eye or severe head trauma in general can cause optic neuropathy. Concussive blows to the head and traumatic brain injury can lead to vision problems including loss or reduction of field of vision, double vision, blurred vision, sensitivity to light, and pain during eye movements. Various types of eye specialists, optometrists, and ophthalmologists are highly and specifically trained to determine concussion symptoms and traumatic brain injuries that may affect an individual’s vision. Anyone who has received a strong blow to the eye and/or head and experiences a loss of vision or any of the symptoms listed above can and should be treated by one of these specialists to determine the severity of the symptoms and possible other damage. Treatments for concussions and brain injuries vary based on the type and degree of symptoms.
Inflammation and Autoimmune Conditions: Inflammation of the optic nerve, or optic neuritis, due to autoimmune conditions will often cause optic neuropathy and severe vision problems. Two of the most common conditions responsible for vision loss are multiple sclerosis and neuromyelitis optica. Multiple sclerosis (or MS) is an autoimmune condition that occurs when nerve endings, including the optic nerve, are damaged due to the immune system attacking the myelin - the substance which is used to cover the trunks of the nerves. MS is one of the most common causes of optic neuritis, and the detection of optic neuritis during eye exams is often an early indicator of the condition. Damage to the optic nerve causes a wide variety of symptoms from blurry or hazy vision, defects of central visual field, dimming of the eyesight and low contrast.
Neuromyelitis optica is another autoimmune disorder in which the immune system primarily attacks the optic nerve, spinal cord, and in some cases, the brain. Its effects on vision are similar to MS, causing optic neuritis and loss of vision. However, neuromyelitis optica, unlike MS, generally has no progressive stage, but rather occurs in repeated acute attacks that can often be even more devastating than those occurring with MS.
Optic neuritis can be detected using standard eye exams like visual field tests or imagining of the optic nerve and more specialized exams like MRI or comprehensive blood tests. Treatment for the condition generally centers around oral steroids which serve an anti-inflammatory purpose.
Non-Development of the Optic Nerve (Optic Nerve Hypoplasia): Optic nerve hypoplasia (or ONH) is a congenital condition resulting from the non-development or underdevelopment of the optic nerve, where the fibers making up the optic nerve either fail to develop or develop incompletely. ONH most commonly affects both eyes, however it can also be present in one eye only. Depending on the severity of the case, NHO can affect vision minimally or drastically, with latter cases involving severe loss of vision and intense difficulties perceiving light due to a reduced numbers of optic fibers. ONH is diagnosed via examination conducted by an ophthalmologist, where the optic nerve will appear structurally abnormal and smaller than a healthy nerve. Treatment of ONH is difficult, and often includes typical assistance for the visually impaired along with treatment of other non-visually related symptoms of the condition.
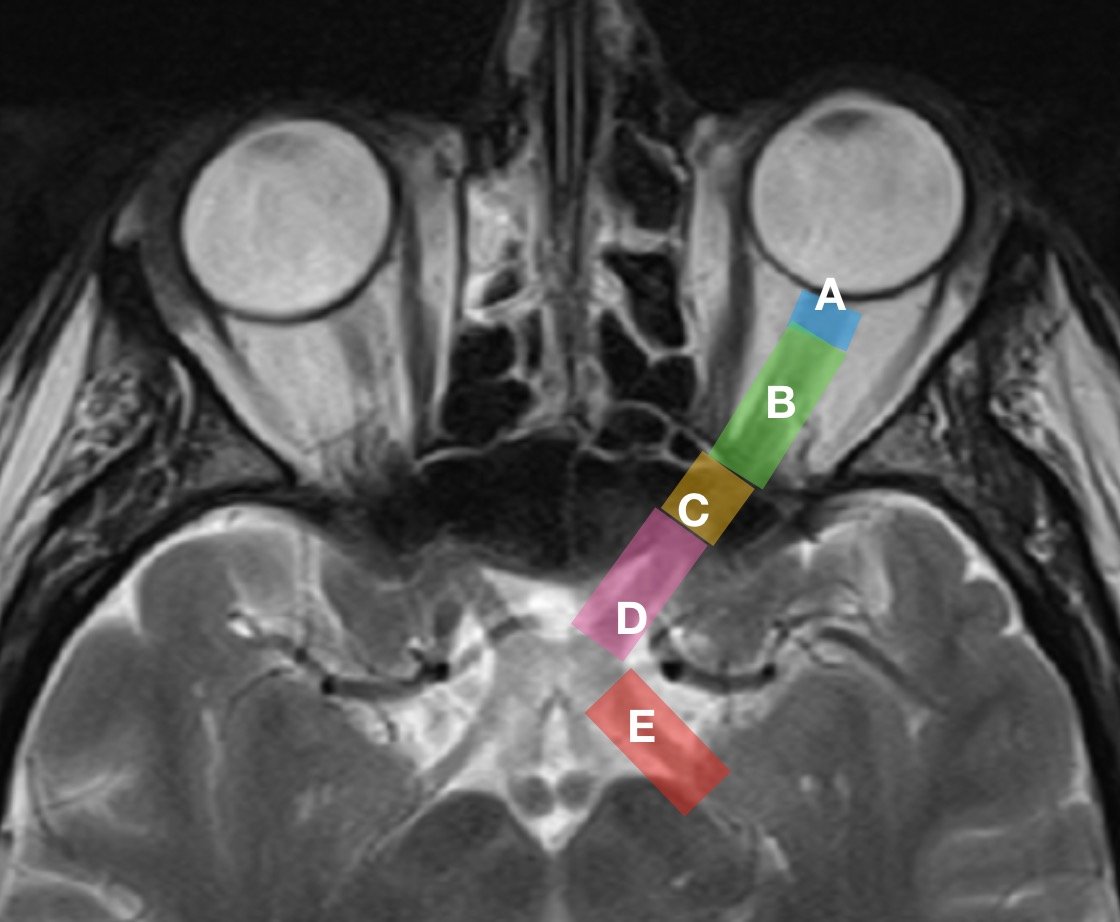
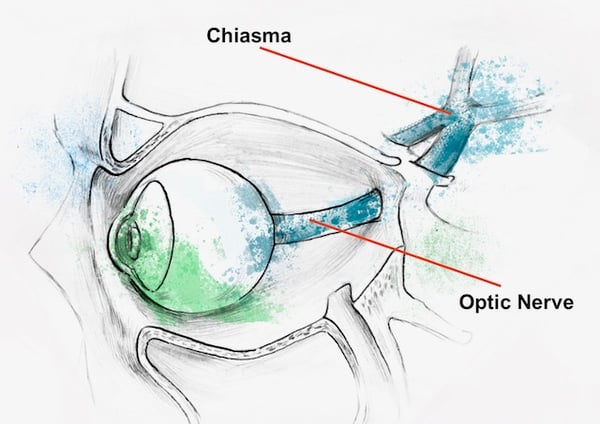
Brain Tumors: Brain tumors can often cause compression of the optic nerve leading to varying degrees of vision loss and different forms of visual impairment. The compression primarily causes local ischemic damages in the optic nerve leading to optic nerve atrophy and disruption of the visual pathway, essentially cutting off the relaying of visual signals from the eyes to the brain. The most typical clinical signs brain tumors are damages to and defects in the field of vision, which can be partial in some areas. In the most severe cases, compete blindness occurs.
One such example of compression occurs in the form of a pituitary adenoma, a type of tumor occurring on the pituitary gland. This form of tumor while growing applies pressure to the optic nerves where they are crossed at the optic chiasm. For this reason, defects of peripheral vision are progressive, starting from the very periphery and slowly damaging more and more side vision. In the end stages, half of the field of vision is gone, a condition better known as bitemporal hemianopia.
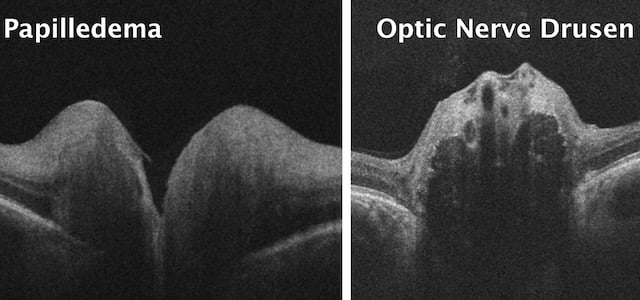
Elevated Intracranial Pressure: Intracranial pressure, or pressure inside the skull, can also cause optic neuropathy. While increased pressure can occur for a number of reasons, it is often caused by brain tumors or conditions such as hydrocephalus, a condition in which cerebrospinal builds up within the brain. If pressure within the skull becomes too high and/or lasts too long, partial or even total blindness can occur. Both hydrocephalus and tumors are generally treated with surgery to reduce a variety of negative symptoms, including vision-related symptoms including blurry vision, double vision, and other visual impairments and disturbances that vary in severity.
Infections and Related Diseases: Different infections can cause optic nerve damage as well, depending on the type and location. Sinusitis (commonly known as a sinus infection), for example, is the inflammation of the sinuses, areas surrounding the nasal cavity that are filled with air. When these become inflamed, severe facial pressure often occurs, particularly between and behind the eyes, causing severe pain and making vision difficult at times. Generally, blurring of vision occurs, although in severe and chronic cases optic neuropathy can occur as well, leading to loss of vision.
Diseases such as lupus and sarcoidosis are other examples of diseases that may have dire effects on vision, particularly the optic nerve. Such infections and diseases are often treated with anti-inflammatory medicines such as steroids, or through antibiotics.
Toxins: Toxins, particularly alcohol, tobacco, and drugs can also cause optic nerve damage and lead to partial or severe loss of vision. For example, prolonged alcohol use can cause toxic optic neuropathy with long-term loss of central vision, color deficiency, and general loss of vision.
See an Eye Care Specialist
In conclusion, if you have experienced any of the symptoms described above, or if you’re worried you may have vision loss or problems related to the causes discussed here, make an appointment with an eye care specialist near you. Many of these symptoms and conditions can cause permanent damage and threaten the future integrity of your vision. If a confirmation of optic nerve damage is made by a professional, make an appointment as soon as possible at the Fedorov Restore Vision Clinic, where you may receive vision restoration therapy.

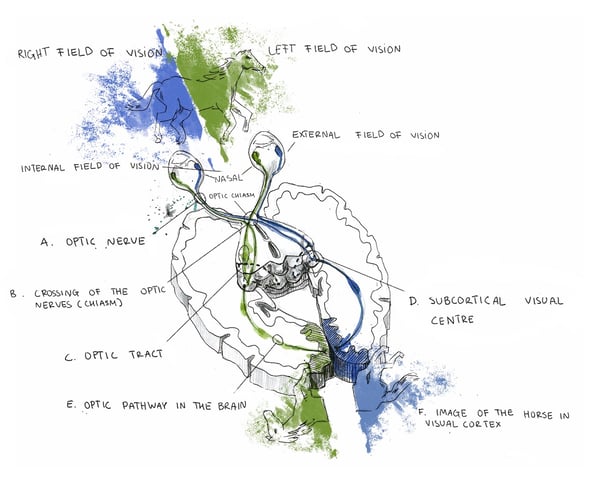 Within the eye is the retina, the cells of which are responsible for perceiving, processing, and relaying information to the brain, where the decoding of the received signals takes place and our actual visual experience occurs. The eye and brain are intricate, complexly structured organs, and their function in the visual process can’t be performed correctly if they’re not properly connected to each other. This is why the optic nerve, acting as a type of bridge between the two, plays such a critical role in how we see the world.
Within the eye is the retina, the cells of which are responsible for perceiving, processing, and relaying information to the brain, where the decoding of the received signals takes place and our actual visual experience occurs. The eye and brain are intricate, complexly structured organs, and their function in the visual process can’t be performed correctly if they’re not properly connected to each other. This is why the optic nerve, acting as a type of bridge between the two, plays such a critical role in how we see the world.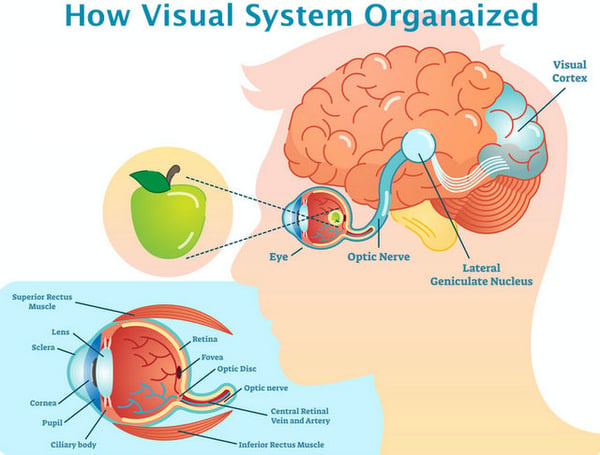













 Blurry vision is often associated with refractive errors like myopia and hyperopia (nearsightedness and farsightedness, respectively) where objects may only appear blurry at a distance or up close. However, symptoms can also occur at all distances, as is the case with astigmatism. Blurred vision often causes one to squint in order to discern objects clearly, causing debilitating headaches and/or eyestrain. But blurry vision can be indicative of several different causes and ailments, and can be difficult to describe or may overlap or be confused with similar symptoms; eye care specialists will often have patients explain just what they mean by “blurry” during examinations. Blurry vision can be symptomatic of common and highly treatable conditions, but may also indicate the presence of more severe conditions as well, such as optic nerve or retinal structural abnormality. If your optician or optometrist cannot treat your blurry vision with corrective lenses, seek care immediately.
Blurry vision is often associated with refractive errors like myopia and hyperopia (nearsightedness and farsightedness, respectively) where objects may only appear blurry at a distance or up close. However, symptoms can also occur at all distances, as is the case with astigmatism. Blurred vision often causes one to squint in order to discern objects clearly, causing debilitating headaches and/or eyestrain. But blurry vision can be indicative of several different causes and ailments, and can be difficult to describe or may overlap or be confused with similar symptoms; eye care specialists will often have patients explain just what they mean by “blurry” during examinations. Blurry vision can be symptomatic of common and highly treatable conditions, but may also indicate the presence of more severe conditions as well, such as optic nerve or retinal structural abnormality. If your optician or optometrist cannot treat your blurry vision with corrective lenses, seek care immediately. Constant eye strain causes squinting, severe discomfort and headaches, just as with blurry vision. However, cloudy vision is different from blurry vision in that it seems as if one is peering through a thick haze or fog, or that one’s vision is “milky”, obscuring objects even further. Hazy or foggy vision can also be indicative of numerous acute or chronic conditions, both common and severe, such as glaucoma, cataracts, and acute optic nerve damage. It is one of the most typically reported symptoms among those suffering from problems with their eyesight, and can be distinguished during routine eye examinations.
Constant eye strain causes squinting, severe discomfort and headaches, just as with blurry vision. However, cloudy vision is different from blurry vision in that it seems as if one is peering through a thick haze or fog, or that one’s vision is “milky”, obscuring objects even further. Hazy or foggy vision can also be indicative of numerous acute or chronic conditions, both common and severe, such as glaucoma, cataracts, and acute optic nerve damage. It is one of the most typically reported symptoms among those suffering from problems with their eyesight, and can be distinguished during routine eye examinations.%20Fedorov%20Restore%20Vision%20Clinic.jpg?width=600&name=Central%20scotoma%20(VF%20defect)%20Fedorov%20Restore%20Vision%20Clinic.jpg) Scotoma is caused by the damage of central fibers of the optic nerve, and frequently occurs in cases of optic neuritis and other autoimmune or inflammatory processes. Major complaints include severe difficulties with straight-ahead sight due to central vision being blurry, foggy, or entirely absent in the form of a blank area (as in the case of total scotoma). In the early stages of developed scotoma, another common complaint includes difficulties in distinguishing colors, especially between light or dark colors.
Scotoma is caused by the damage of central fibers of the optic nerve, and frequently occurs in cases of optic neuritis and other autoimmune or inflammatory processes. Major complaints include severe difficulties with straight-ahead sight due to central vision being blurry, foggy, or entirely absent in the form of a blank area (as in the case of total scotoma). In the early stages of developed scotoma, another common complaint includes difficulties in distinguishing colors, especially between light or dark colors. Most noticeable defects occur in the bottom of the field of vision, or the nasal or temporal parts. Depending on the severity of the case, patients describe their condition as partial loss, where the field of vision is not completely lost, but rather becomes low-functioning, with the individual experiencing hazy or blurry vision on the periphery. In severe cases peripheral vision is entirely absent. Extremely severe conditions such as advanced or terminal glaucoma leave only limited central vision preserved.
Most noticeable defects occur in the bottom of the field of vision, or the nasal or temporal parts. Depending on the severity of the case, patients describe their condition as partial loss, where the field of vision is not completely lost, but rather becomes low-functioning, with the individual experiencing hazy or blurry vision on the periphery. In severe cases peripheral vision is entirely absent. Extremely severe conditions such as advanced or terminal glaucoma leave only limited central vision preserved.  This is called “tunnel vision”, which means that central vision may remain intact and function normally, leading to the effect of seeing things through a tunnel or tube.
This is called “tunnel vision”, which means that central vision may remain intact and function normally, leading to the effect of seeing things through a tunnel or tube.  Due to excessively bright light, poor visibility and poor visual performance is observed. In addition, recovery time from bright lights is longer than typically experienced. Glare is generally caused by an inability of photoreceptor cells in your retina to focus light received from your environment, and also depends on damaged retinal ganglion cells in the case of optic neuropathy. Glare is often described by patients as causing a “shimmer” or “halo” effect when trying to focus on a light-reflecting object or area in one’s field of vision. Like many other symptoms of neuropathy, this can cause one to squint while attempting to focus, causing painful eyestrain and headaches. Finally, glare can be caused by any condition affecting the retina and photoreceptor cells, and can be indicative of serious eye conditions.
Due to excessively bright light, poor visibility and poor visual performance is observed. In addition, recovery time from bright lights is longer than typically experienced. Glare is generally caused by an inability of photoreceptor cells in your retina to focus light received from your environment, and also depends on damaged retinal ganglion cells in the case of optic neuropathy. Glare is often described by patients as causing a “shimmer” or “halo” effect when trying to focus on a light-reflecting object or area in one’s field of vision. Like many other symptoms of neuropathy, this can cause one to squint while attempting to focus, causing painful eyestrain and headaches. Finally, glare can be caused by any condition affecting the retina and photoreceptor cells, and can be indicative of serious eye conditions. Objects appear darker and less clear than they are in actuality, which can also make them appear blurry, hazy, or lacking proper contrast.
Objects appear darker and less clear than they are in actuality, which can also make them appear blurry, hazy, or lacking proper contrast.


 Note: The information given in this blog are the opinions of the authors and for reader familiarization purposes only. This blog is not intended as a substitute for professional medical advice. Also, the information provided does not replace or abolish any official or legal terms for glaucoma diagnosis, treatment, and management. Authors are not liable for any undesirable consequences or effects related to the information provided in the blog.
Note: The information given in this blog are the opinions of the authors and for reader familiarization purposes only. This blog is not intended as a substitute for professional medical advice. Also, the information provided does not replace or abolish any official or legal terms for glaucoma diagnosis, treatment, and management. Authors are not liable for any undesirable consequences or effects related to the information provided in the blog.